In a nutshell
- researchers discover an unexpected target of a leukemia drug, explaining its side effects
- the novel target could provide an opportunity for repurposing the drug to treat other diseases
Side-effects of leukaemia drug explained, reveal possibility of repurposing to treat other diseases
By tracking the impact of a widely used leukaemia drug on proteins inside living cells, research led by EMBL and Cellzome has shed light on the molecular causes of the drug’s side effects. Published in Nature Chemical Biology, the study also indicates that the drug has potential to be repurposed to treat tyrosinemia, a rare genetic disorder that can lead to liver, kidney and neurological problems.
Many drugs used in the treatment of cancer have severe side effects. These occur when the drugs affect not only the target proteins in tumour cells, but also proteins in healthy cells. By identifying proteins that are inadvertently targeted by anti-cancer drugs, scientists aim to learn more about who might be affected, how and why, in order to better inform treatment.
Warming up
Two years ago, at drug discovery company Cellzome, an international team led by Mikhail Savitski developed an elegant method known as thermal proteome profiling, which they believe can provide answers to such puzzles. By heating up cancer cells, the technique enables researchers to compare the ‘melting’ behaviours of individual proteins before and after the administration of a cancer drug, ultimately revealing which proteins the drug is targeting.
“After we developed this technology I could not stop thinking about ways to develop it and apply it in different settings – it opens up some very exciting research paths,” explains Savitski, who joined EMBL as a group leader this year.
Sidetracked
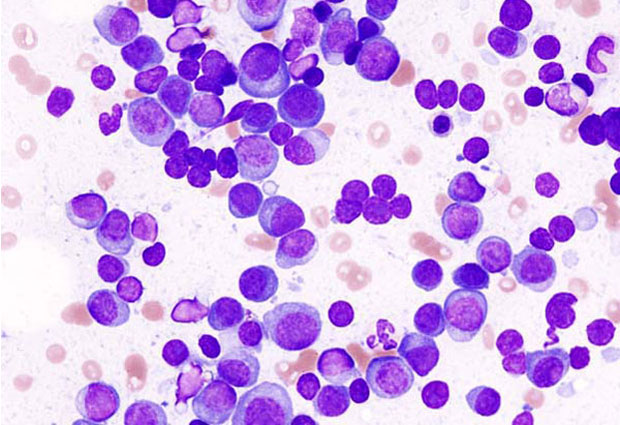
One of these paths emerged out of the blue. The team were developing a refined version of the technology using a drug for multiple myeloma – a type of leukaemia that affects plasma cells. In some patients, the drug, panobinostat, causes a variety of serious side effects, including hyperthyroidism.
In the study, Savitski and colleagues identified an unexpected target of the drug: a protein called phenylalanine hydroxylase (PAH). As its name implies, PAH acts on phenylalanine. Phenylalanine is an amino acid, one of the building blocks proteins are made of, so it is essential for life. But too much phenylalanine can lead to problems including neurological damage and hyperthyroidism. Since PAH’s job in the cell is to convert phenylalanine into another amino acid – tyrosine – this explained how panobinostat can cause hyperthyroidism. The leukaemia drug inadvertently targets PAH, phenylalanine is not converted to tyrosine as it should be, so it accumulates in a patient’s cells. “Our study underscores the importance of monitoring amino acid levels in patients and the need to take caution when applying the drug,” says Marcus Bantscheff, head of technology at Cellzome, who co-led the study.
The research, which was supported by colleagues from Utrecht University and the University of Texas Health Science Center, also identifies panobinostat as the first drug capable of inhibiting PAH, opening up potential avenues for repurposing it to tackle other illnesses. “It could provide an opportunity to develop treatments for diseases where PAH plays a big role, such as tyrosinemia,” adds Isabelle Becher, the first author of the study. “The study provides an ideal starting point from which one can look to develop a drug that is really specific.”
SOURCE ARTICLE
This article was originally published on EMBL News
